Many people assume that hormonal birth control has a single function to prevent pregnancy. Although hormonal contraceptives are generally more effective than barrier or lifestyle-based methods, their impact extends beyond simply avoiding pregnancy. These methods influence the body in various ways and can produce both beneficial and adverse effects. While different types of hormonal birth control tend to share similar advantages and potential risks, individual responses to the hormones can vary significantly from person to person. This study seeks to highlight and examine the potential risks associated with the use of hormonal contraceptive methods, with the goal of increasing awareness and understanding of their broader effects.
Anxiety: A review published in 2004 reported that individuals who used hormonal birth control tended to experience higher levels of anxiety compared to those who did not use hormonal contraceptive methods. These findings suggest a possible connection between hormone-based contraception and mental health changes. Further reinforcing this association, a 2018 study found that people using hormonal intrauterine devices (IUDs) also showed increased rates of anxiety, indicating that the effect is not limited to one specific type of hormonal contraceptive.
Certain hormonal methods appear to be more strongly linked to mood-related side effects than others. In particular, combined oral contraceptive pills, which contain synthetic forms of both estrogen and progesterone, as well as progestin-only minipills, have been associated with higher rates of depression and anxiety when compared to non-hormonal or alternative contraceptive methods. Research suggests that between 4% and 10% of users of combined pills report experiencing negative mood changes, such as increased irritability, sadness, or emotional instability, during use.
Depression: A study published in 2023 suggested that individuals who use oral contraceptive pills may experience a significantly higher risk of developing depression, with the risk increasing by as much as 130%, particularly during the first two years after beginning use. One of the most extensive and influential investigations on this subject was carried out in Denmark in 2016. In this large-scale study, researchers examined 14 years of health data from more than one million women between the ages of 15 and 34. To reduce potential bias, the study excluded individuals who had a prior history of depression or had previously used antidepressant medications.
Using this data, researchers estimated that approximately 2.2% of people who started using hormonal birth control were prescribed antidepressants within their first year of use, compared to 1.7% of individuals who were not using any form of hormonal contraception. The findings also showed that users of hormonal intrauterine devices (IUDs) were about 1.4 times more likely to be prescribed antidepressants than non-users of hormonal birth control, with the increased risk being particularly noticeable among adolescents and young adults aged 15 to 19.
Breakthrough bleeding: refers to unexpected spotting or bleeding that occurs outside of a regular menstrual period, especially when using hormonal birth control. A 2016 review found that about 30% to 50% of people using combined oral contraceptive pills experience breakthrough bleeding during the first three to six months of use. As the body adjusts to the hormones, the occurrence of this bleeding usually decreases, dropping to about 10% to 30% by the third month. Breakthrough bleeding is more common among users of continuous or extended-cycle pills and is also the most frequently reported side effect of the progestin-only minipill. While it is often linked to birth control pills, breakthrough bleeding can occur with all hormonal contraceptive methods, as they can affect the timing, amount, and length of period-like bleeding. In most cases, these changes improve over time as the body becomes accustomed to the hormones.
Stress: A study published in 2023 indicated that the use of oral contraceptive pills may interfere with the body’s natural stress response, potentially making it more difficult for individuals to effectively cope with and adapt to stressful situations. According to the findings, hormonal changes caused by the pill may alter how the body reacts when exposed to stressors. The study also reported that individuals using the pill showed higher levels of the inflammatory cytokine tumor necrosis factor–alpha (TNF-alpha) both before and after undergoing a stress test. This elevation in TNF-alpha suggests an increase in inflammation and may be associated with a stress response pattern that more closely resembles what is typically observed in males. These results highlight the possibility that hormonal contraceptives can influence not only reproductive health but also immune function and stress regulation.
In contrast, individuals with natural menstrual cycles exhibited higher levels of interleukin-6, a cytokine commonly associated with a more “female-typical” stress response. This difference highlights how hormonal contraceptives may shift the body’s immune and stress-related signaling pathways. Additionally, the pill may reduce the body’s natural production of progesterone, a hormone that is normally converted into allopregnanolone. Allopregnanolone is known for its calming and anxiety-reducing effects on the brain, and lower levels of this hormone may further contribute to altered stress regulation and emotional responses among pill users. Together, these findings suggest that oral contraceptives can influence not only reproductive hormones but also stress adaptation, immune function, and emotional well-being.
Headache and Migraine: Research has identified a connection between the use of hormonal birth control and an increased occurrence of headaches and migraine episodes. Fluctuations in estrogen levels throughout the menstrual cycle are known to trigger menstrual migraines in some individuals. Because hormonal contraceptives can modify the body’s natural estrogen patterns, they may contribute to the development or worsening of headaches and migraines in certain users.
For individuals who have a history of migraine with aura, combined hormonal birth control methods which contain estrogen may pose additional risks. Healthcare professionals often advise against the use of these contraceptives in such cases, as elevated estrogen levels have been associated with an increased risk of stroke. As a result, people with migraine with aura are typically encouraged to discuss alternative, non-estrogen-containing contraceptive options with their healthcare provider to reduce potential health risks.
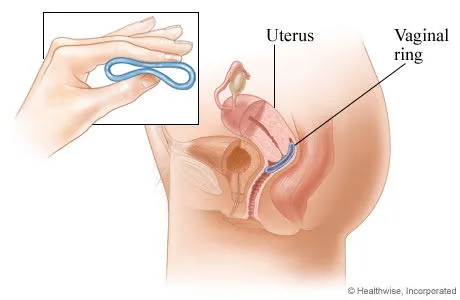
Decreased Libido: Hormonal birth control has been linked to a variety of physical side effects, such as fatigue, nausea, irregular bleeding, and cramping, which can indirectly or directly affect sexual desire and overall libido. Changes in hormone levels may also create conditions that reduce sexual interest or arousal. For instance, some individuals experience vaginal dryness, discomfort or pain during penetration, and decreased sensitivity, all of which can negatively influence sexual experiences. A 2013 review of 36 studies examining sexual desire among users of combined oral contraceptive pills found that out of 8,422 participants, 1,238 individuals (15%) reported a decrease in libido. In contrast, 1,826 participants (21%) experienced an increase in sexual desire, while the majority reported no noticeable change. Further evidence from a 2016 review of 103 studies on birth control and sexuality highlighted several positive sexual outcomes associated with certain contraceptive methods. The review noted that hormonal IUDs may reduce pain during intercourse and increase libido after about a year of use. Both hormonal and nonhormonal (copper) IUDs were found to potentially enhance libido, physical arousal, sexual satisfaction, and the frequency of sexual activity. Additionally, the vaginal ring has been associated with improvements in libido, arousal, sexual satisfaction, vaginal lubrication, and orgasm quality. The contraceptive implant was also linked to positive effects, including increased arousal, sexual satisfaction, and improved orgasm, along with reduced pain during sex and decreased anxiety related to sexual activity.
Vaginal Discomfort: A reduction in libido can make it more challenging for an individual to become physically aroused, which may in turn lead to decreased natural vaginal lubrication. When arousal is diminished, the body may not produce sufficient lubrication, potentially causing discomfort during sexual activity. Supporting this, a study published in 2023 found that the use of oral contraceptive pills may reduce blood flow to the genital region. This decreased circulation can further limit the body’s ability to produce adequate lubrication, thereby contributing to dryness and reduced sexual comfort. These findings suggest that hormonal birth control may influence sexual functioning not only through changes in desire but also through physiological effects on arousal and blood flow.
Ovarian Cysts: While hormonal birth control is generally known to reduce the risk of developing ovarian cysts, some intrauterine devices (IUDs) may actually have the opposite effect. Research indicates that certain hormonal IUDs are associated with a higher likelihood of cyst formation. For example, approximately 22 out of every 100 individuals (22%) using the Kyleena IUD develop an ovarian cyst, whereas around 14 out of 100 users (14%) of the Skyla IUD experience the same. Other hormonal IUDs show somewhat lower rates: about 7.5% of Mirena users and 4.7% of Liletta users develop ovarian cysts. These statistics highlight that while hormonal IUDs offer effective contraception, they may also carry specific risks related to ovarian health, which vary depending on the type of device used.
Stroke: According to the American College of Cardiology, the risk of experiencing a stroke while using combined oral contraceptive pills is generally lower than the risk of having a stroke related to pregnancy. This suggests that, although there is some level of risk associated with these contraceptives, it remains comparatively smaller than the risks encountered during pregnancy. Supporting this, a 2019 meta-analysis of multiple studies found that the risk of both ischemic stroke and overall stroke increases by approximately 20% for every 10 micrograms of estrogen contained in the pill, as well as for every additional five years of use. These findings indicate that while combined hormonal contraceptives are highly effective for preventing pregnancy, their estrogen content and duration of use can influence cardiovascular risk, emphasizing the importance of individualized medical guidance when choosing a contraceptive method.
Hypertension: The use of combined hormonal contraceptives, such as the pill, patch, and vaginal ring, has been shown to potentially raise blood pressure in some individuals. This increase in blood pressure may contribute to a higher risk of cardiovascular complications over time, particularly in those who already have hypertension or other underlying risk factors. In contrast, the contraceptive injection, often referred to as the shot, does not appear to have a significant effect on blood pressure. However, it may lead to elevated cholesterol levels, which is another important factor that can contribute to cardiovascular disease. These differences highlight that while all hormonal contraceptives can impact cardiovascular health to some degree, the specific risks vary depending on the type of method used, underscoring the importance of discussing personal health history with a healthcare provider when selecting a birth control option.
Natural ways for birth control
Tracking ovulation is a way to understand your fertility and reduce the risk of pregnancy by identifying the days you are most likely to conceive. Pregnancy is most likely around the time an egg is released from the ovary, which can be fertilized for about 24 hours, while sperm can survive in the reproductive tract for up to five days. Several methods can help track fertility.
The Rhythm Method requires monitoring your menstrual cycles for 6–12 months and using calculations to identify your first and last fertile days. The Standard Days Method simplifies this by designating days 8 through 19 as fertile for anyone with a cycle length between 26 and 32 days, making it easier to track with a calendar, app, or color-coded beads.
The Cervical Mucus Method involves observing changes in cervical mucus, which increases in volume and becomes clear, slippery, and stretchy during ovulation. Tracking these patterns over time can help predict fertile days.
The Basal Body Temperature Method involves recording your temperature daily with a basal thermometer. A slight rise in temperature can indicate ovulation, but factors like illness, stress, alcohol, travel, or changes in sleep can affect accuracy.
The Withdrawal Method, or “pulling out,” requires removing the penis before ejaculation, but it has a high failure rate of around 22%, making it less reliable. Some herbs, including neem, castor bean, turmeric, gossypol, and wild carrot, are sometimes promoted as natural contraceptives, but there is little scientific evidence supporting their effectiveness, and some can be harmful, so medical advice is recommended before using them.
It’s important to note that methods based on calendar tracking, mucus observation, or basal temperature are much less reliable for individuals with irregular cycles caused by conditions like thyroid disorders, eating disorders, significant weight changes, excessive exercise, or certain medications and lifestyle factors. Combining methods or consulting a healthcare provider can improve accuracy and help you make safe, informed choices about pregnancy prevention